The Great Alzheimer’s Scam and The Proven Cures They’ve Buried for Billions
October 6 | Posted by mrossol | Health, MedicineDecades of neglect in understanding the actual causes of dementia have transformed it into one of the most costly diseases in existence.
Source: The Great Alzheimer’s Scam and The Proven Cures They’ve Buried for Billions
• Alzheimer’s disease is commonly thought to result from abnormal plaque buildup in the brain that gradually destroys brain tissue. As a result, almost all Alzheimer’s research has been directed toward eliminating amyloid, even after the basis for much of this work was shown to stem from fraudulent research.
•As such, despite decades of research and billions of dollars spent, this model has completely failed to produce useful results. The costly “groundbreaking” Alzheimer’s drugs only slightly slow dementia progression—at the expense of causing brain bleeding and swelling in over a quarter of those treated.
•In contrast, numerous affordable treatments have been developed for Alzheimer’s disease that target the root causes of the disorder, producing significant benefits at a fraction of the cost and without any toxicity.
•One neurologist, for example, proposed that amyloid serves a protective function in the brain and treats Alzheimer’s by identifying the underlying process causing dementia (which can often be diagnosed through symptoms). Remarkably, despite the method being proven in clinical research, awareness of it or the fact there are completely different types of “Alzheimer’s disease” which require different treatments remains almost nonexistent.
•Likewise, a strong case can be made that impaired cerebral circulation, along with impaired venous and lymphatic drainage, plays a pivotal role in Alzheimer’s disease.
•This article will review the common causes of cognitive impairment and dementia (e.g., cells becoming trapped in a shocked state where they no longer function) along with the forgotten treatments for neurodegenerative disorders—some of which, like DMSO, have extensive evidence supporting their use.
One of the least appreciated aspects of medicine is the numerous frameworks that have been developed to understand how the body works and how to heal it. This, I believe is a result of conventional medicine having successfully branded itself as the one true path to understanding the body and each remaining approach being a “second-rate gimmick,” which at best, can sometimes assume a complementary role in healthcare.
However, if you study those other approaches, you will find each medical system excels at certain types of health problems, while struggling with others, so in many instances, knowing which medical model to jump to can be immensely beneficial to patients.
The modern approach to medicine is heavily biased towards a biochemistry model, where customized drugs are designed to stimulate or inhibit specific molecular targets (most commonly enzymes, frequently cellular receptors or ion channels, and less often, other aspects of the body, such as individual genes or inflammatory messengers). This approach, in turn, tends to excel for specific issues (particularly acute emergencies) but typically struggles with chronic ailments—something I attribute both to target molecules rarely being able to reach broad swathes of the body and partly due to living organisms being designed to adapt to excessive stimulation or inhibition of specific receptors and enzymes within the body.
Yet despite its frequent failures, we continue to rigidly adhere to that model of medicine. This I believe, ultimately is because therapies produced within this framework are highly specific to individual diseases (hence allowing many distinct patentable products), and in many cases (since they can only temporarily shift an enzyme or receptor) do not produce lasting cures—hence requiring perpetual purchases of them and thus recurring pharmaceutical sales.
Note: in many cases, disabling critical enzymes or receptors also creates a myriad of side effects (particularly over time as the body readjusts itself to accommodate this unnatural state).
All of this summarizes why, despite spending an ever increasing amount of money on Alzheimer’s research (e.g., the NIH spent 2.9 billion in 2020 and 3.9 billion in 2024), we have still failed to make any real progress on the disease. Furthermore, we only spend that much money on Alzheimer’s research because of how dire its costs are (e.g., last year it was estimated to cost the United States 360 billion dollars). Sadly, this figure only touches the surface of the social cost (as any relative of someone with Alzheimer’s can attest)—again making it so remarkable we still have not made any progress in the illness.
The Amyloid Juggernaut
The early history of Alzheimer’s research is as follows: In 1906, plaques in the brain were identified as the cause of Alzheimer’s disease, in 1984, amyloid beta protein was identified as the primary component of those plaques, and in 1991, genetic mutations in a protein that gives rise to amyloid beta was linked to inherited forms of Alzheimer’s disease—creating a widespread believe a cure for this devastating disease was at last at hand.
The existing dogma within Alzheimer’s research, hence, became that Alzheimer’s disease results from the buildup of amyloid plaques within the brain, which then cause brain damage that leads to Alzheimer’s disease. As such, the majority of research for treating Alzheimer’s disease has thus been targeted at eliminating these plaques, but unfortunately:
Hundreds of clinical trials of amyloid-targeted therapies have yielded few glimmers of promise, however; only the underwhelming Aduhelm has gained FDA approval. Yet Aβ still dominates research and drug development. NIH spent about $1.6 billion on projects that mention amyloids in this fiscal year, about half its overall Alzheimer’s funding. Scientists who advance other potential Alzheimer’s causes, such as immune dysfunction or inflammation, complain they have been sidelined by the “amyloid mafia.” Forsayeth says the amyloid hypothesis became “the scientific equivalent of the Ptolemaic model of the Solar System,” in which the Sun and planets rotate around Earth.
Note: frequently, when a faulty paradigm fails to explain the disease it claims to address, rather than admit the paradigm is flawed, its adherents will label each conflicting piece of evidence as a paradox (e.g., the French “paradox”clearly disproves the cholesterol hypothesis) and dig deeper and deeper until they can find something to continue propping up their ideology. For those interested, the key misunderstandings about cholesterol, heart disease, and statins are discussed here.
The consistent failure of the amyloid model to cure Alzheimer’s gradually invited increasing skepticism towards it, which resulted in more and more scientists studying alternative models of the disease. Before long, they found other factors played a far more significant role in causing the disease (e.g., chronic inflammation), and by 2006, this perspective appeared poised to change the direction of Alzheimer’s research.
In response, the amyloid proponents adopted the position that the shortcoming of their hypothesis was that the cause of Alzheimer’s was not the presence of amyloid plaques in general, but rather the formation of certain toxic oligomers (smaller clumps of amyloid beta). In turn, as dissent towards the amyloid hypothesis was reaching a critical mass, a 2006 paper(published in Nature) identified a previously unknown toxic oligomer, amyloid beta star 56 or Aβ*56, and provided proof that it caused dementia in rats.
This paper cemented both the amyloid beta and toxic oligomer hypotheses (as it provided the proof many adherents to the theory had been waiting for) and rapidly became one of the most cited works in the field of Alzheimer’s research. Its authors rose to academic stardom, produced further papers validating their initial hypothesis, and billions more were invested by both the NIH and the pharmaceutical industry in research of the amyloid and toxic oligomer hypothesis.
It should be noted that some were skeptical of their findings and likewise were unable to replicate this data, but rarely had a voice in the debate:
The spotty evidence that Aβ*56 plays a role in Alzheimer’s had [long] raised eyebrows. Wilcock has long doubted studies that claim to use “purified” Aβ*56. Such oligomers are notoriously unstable, converting to other oligomer types spontaneously. Multiple types can be present in a sample even after purification efforts, making it hard to say any cognitive effects are due to Aβ*56 alone, she notes—assuming it exists. In fact, Wilcock and others say, several labs have tried and failed to find Aβ*56, although few have published those findings. Journals are often uninterested in negative results, and researchers can be reluctant to contradict a famous investigator.
Sound familiar?
Amyloid Scandals
Fifteen years later, at the end of 2021, a neuroscientist physician was hired by investors to evaluate an experimental Alzheimer’s drug and discovered signs that its data consisted of doctored images of Western Blot protein tests(and therefore erroneous assessments of what oligomers were present within research subjects’ brains). As he explored the topic further, he discovered other papers within the Alzheimer’s literature had been flagged by Pubpeer (a website scientists use to identify suspect studies) for containing doctored Western Blots.
Before long, he noticed three of these papers had been published by the same author and decided to investigate their other publications. This led him to the seminal 2006 Alzheimer’s publication, which like the author’s other works, contained clear signs of fraud (again illustrating how criminals typically get caught because they repeated the same crime).
A subsequent investigation uncovered 20 papers written by the author, 10 of which pertained to Aβ*56, and many outside investigators, after being consulted, agreed that the images had been manipulated. A co-researcher came forward, stating that he had previously suspected the author of scientific misconduct (shortly before 2006) and not only withdrew his collaboration with the author but also declined to publish a study they had collaborated on, so he would not potentially be implicated in scientific misconduct.
Note: a major concern with the mRNA vaccines was whether they were stable enough to actually produce their intended product. Since Western Blots are used to demonstrate the presence of proteins, they were presented as proof of vaccine efficacy. When reviewing Pfizer’s regulatory submissions, we discovered that their Western Blots had been fabricated (and hence exposed this in January 2023, as, at the time, provable fraud was one of the few things that could derail the mRNA campaign)—but of course, were completely ignored.
The Amyloid Industry
One of the remarkable things about this monumental fraud was how little was done about it. For example, the physician who discovered it notified the NIH in January 2022, yet in May 2022, beyond nothing being done, the suspect researcher was awarded a coveted $764,792 research grant by the NIH(which was signed off by another one of the authors of the 2006 paper).
In July 2022, Science published an article exposing the incident and the clear fraud that had occurred, after which a few other independent voices attempted to draw attention to it (e.g., I did in October 2022). Despite this, the researcher was allowed to remain in his position as a tenured medical school professor. It was not until June 2024 that the 2006 article was retracted at the request of the authors—all of whom denied being at fault and insisted the doctored images had not affected the article’s conclusions (and likewise the amyloid field claimed this fraud had not refuted the amyloid hypothesis). Eventually, on January 29, 2025, during his confirmation hearing, RFK cited the paper as an example of the institutional fraud and wasted tax dollars within the NIH, and a few days later, that researcher announced his resignation from the medical school professorship (while still maintaining his innocence).
All of this, on the surface, is quite strange and illustrates how much the medical field was willing to walk in lockstep to protect the amyloid hypothesis, something I attribute both to how much many researchers have are dependent upon perpetual funding for it and also how profitable the potential amyloid market is (e.g., roughly 7 million adults have it, many of the therapies cost tens of thousands a year and in theory, they must be covered by Medicare, equating to hundreds of billion in annual sales).
Recently, the fate of the failed amyloid drugs appeared to be changing, as a new pharmaceutical (a monoclonal antibody) demonstrated some success in treating Alzheimer’s—something which was treated as revolutionary by the medical community, the pharmaceutical industry, and drug regulators, as all of them had been waiting for decades for a drug like that to emerge. In turn, the first new drug received accelerated approval (which the FDA proudly announced), due to the controversy surrounding the first one. The second received a quiet backdoor approval, while the third was partially approved a year and a half later.
Each year, Chase Bank holds a private conference for pharmaceutical investors, which sets the tone for the entire industry. In 2023 (the first in-person one since the pandemic), its focus (covered in detail here) was on the incredible profitability of the new Alzheimer’s drugs and the GLP-1s like Ozempic (which the FDA has also relentlessly promoted). While much could be said about the jubilation of that private conference, in my eyes, the most crucial detail was that the (widely viewed as corrupt) FDA commissioner was the keynote speaker, and a few days before the conference, had enacted the second backdoor approval.
However, despite the rosy pictures painted around the drugs (which each attacked different aspects of amyloids), they were highly controversial as:
•The FDA’s independent advisory panel, in a very unusual move, voted 10-0 (with one abstaining) against approving the first amyloid drug (which targeted amyloid plaques), then the FDA approved it anyways. In a highly unprecedented move, three of the advisors resigned, calling it “probably the worst drug approval decision in recent U.S. history.”
•That drug was priced at $56,000 a year—making it sufficient to bankrupt Medicaire, which attracted a Congressional investigation and led to each subsequent one being priced roughly half that amount (along with its price later being reduced to match that).
•Brain swelling or brain bleeding was found in 41% of patients enrolled in its studies. Additionally, headaches (including migraines and occipital neuralgia), falls, diarrhea, confusion, and delirium were also notably elevated compared to placebo.
•No improvement in Alzheimer’s was noted; rather one analysis found it slowed the progression of Alzheimer’s by 20% (although this could have been a protocol artifact rather than a real effect).
The second monoclonal antibody (which targeted amyloid precursors) had a slightly better risk benefit profile (only 21% experienced brain bleeding and swelling), and 26.4% reduction in the progression of Alzheimer’s was detected in the trail (which for context, translated to a 0.45 reduction on a scale where a reduction of at least 1-2 points is needed to create an impact which is in anyway meaningful for a patient).
The third monoclonal (which targeted amyloid plaques thought to be more pathologic) was also contested as it caused 36.8% of recipients to develop brain bleeding or swelling, like the other amyloid medications, frequently caused headaches and infusion reactions (e.g., nausea, vomiting, changes in blood pressure, hypersensitive reactions or anaphylaxis) and there were reasons to suspect the trial had overstated its benefits.
Given the controversy around the first two drugs, the third was met with widespread protest, but in a remarkable pivot, the FDA’s new advisory panel, voted unanimously in favor of it, despite it having a very similar mechanism, efficacy and toxicity to the previously unanimously rejected amyloid drug (which they attributed to it having a better trial design and guidelines for usage). It should hence come as no surprise that when the British Medical Journal conducted an independent investigation, they discovered that within publicly available databases, 9 out of 10 members of the advisory committee had significant financial conflicts of interest.
Note: the tenth individual who voted for the drug, the patient representative, did not exist within those databases and, therefore, could not be assessed.
In short, I believe it is fair to say that the amyloid drugs are effectively failed medications, both due to their side effects and negligible benefits. Fortunately, despite the aggressive promotion of them, despite Chase’s best attempts to promote the sector, the market somewhat recognized how bad they were, as the first drug had its price halved. Then it was withdrawn from the market as no one wanted it (making around 5 million dollars total), while the other two have had very modest sales (e.g., 295 million for the most popular one).
From this, three things stand out:
•These drugs consistently damaging brain tissue indicated either that their mechanism of action (triggering the brains immune cells to attach amyloids) would cause those immune cells also to attack the brain or that removing amyloid (regardless of the way it was done) damages brain tissue (suggesting amyloid has a protective effect for the brain) and damages brain blood vessels (e.g., because the amyloids patch vessel walls)—either of which strongly argues against the approach. Curious, I checked, and there indeed is evidence for all three of those occurring (and an active subject of discussion)—yet it has not deterred the usage of this therapy.
•An absolutely absurd amount of money and time has been wasted on this endeavor due to the medical field’s need to find a patentable drug.
•The focus on these lucrative drugs has diverted attention from other treatments that are more likely to help Alzheimer’s patients. In turn, the entire reason I wrote this article is because those treatments do indeed exist, and the harm from withholding them has been incalculable.
For example, after I posted a few articles about Alzheimer’s early in this publication’s history, I had numerous readers reach out to share that coconut oil, or coconut oil-derived MCTs, had significantly improved an ailing relative’s dementia. I checked, and found a randomized controlled trial that over 6 months, found 80% remained stable or improved—which for context, is better than what any of the amyloid drug trials showed, and more importantly, does not cause brain bleeds and costs a lot less than the annual (approximately) $30,000 cost for those drugs. I share this, not to claim coconut oil is the cure for dementia, but rather to highlight just how much the data from these drugs have been overvalued to create a new drug market.
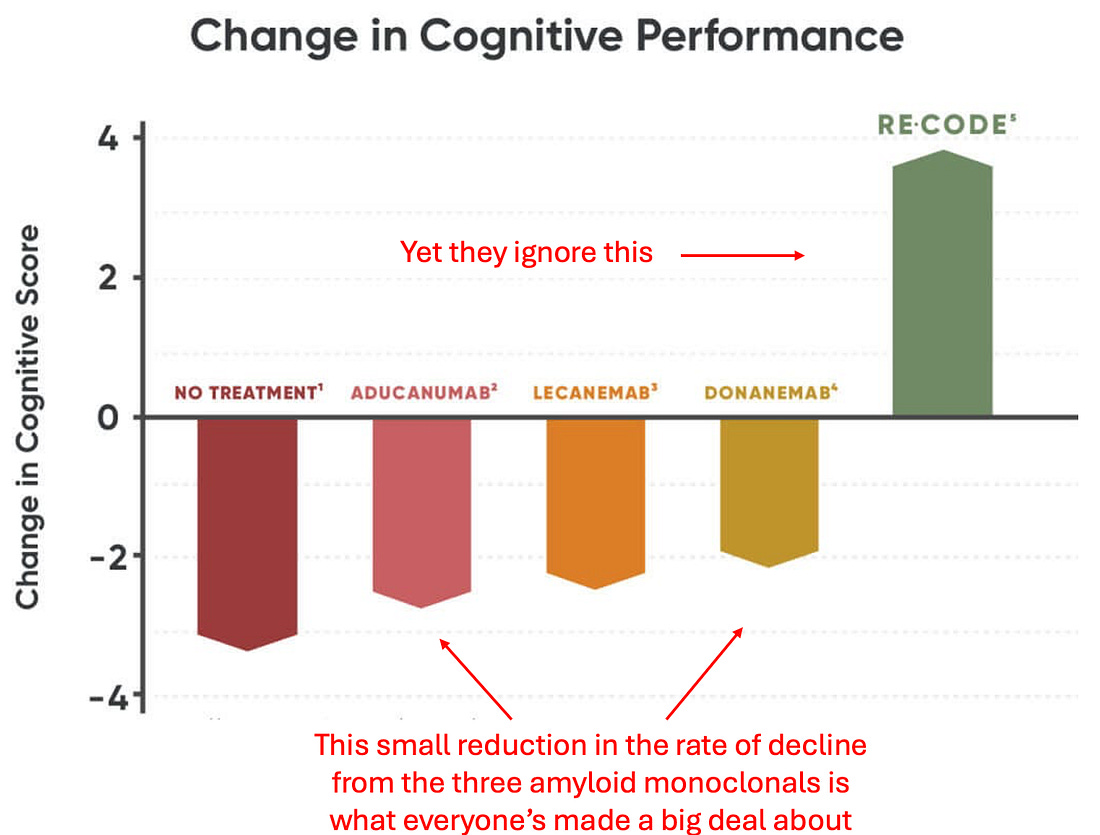
Likewise, very few are aware of a 2022 study that should have revolutionized the entire Alzheimer’s field:
Note: Bredesen’s references for the above chart can be found here, here, and here.
Dale Bredesen’s Discovery
Dale Bredesen is a creative neurologist with a background in functional medicine who spent several years examining the Alzheimer’s question. From it, as detailed in The End of Alzheimer’s, he reached a few pivotal conclusions:
•Amyloid protein is a protective mechanism the brain uses to protect itself from other stressors that endanger brain tissue.
•Rather than there being one type of Alzheimer’s, there are actually three with different symptoms, and it is essential to recognize which type someone has before initiating treatment.
•The brain is designed to be able to adapt to the needs of life, so it is always creating or pruning neural connections and brain cells. Alzheimer’s, in turn, results from the loss of signals that sustain brain cells, and the dismantling of neural connections outweighing the formation of new ones, gradually compounding over the decades.
As such, his formula was fairly straightforward: identify the type of Alzheimer’s someone has, eliminate its causes, and gradually wait for the physiological momentum to shift from neurodegeneration to neurodevelopment.
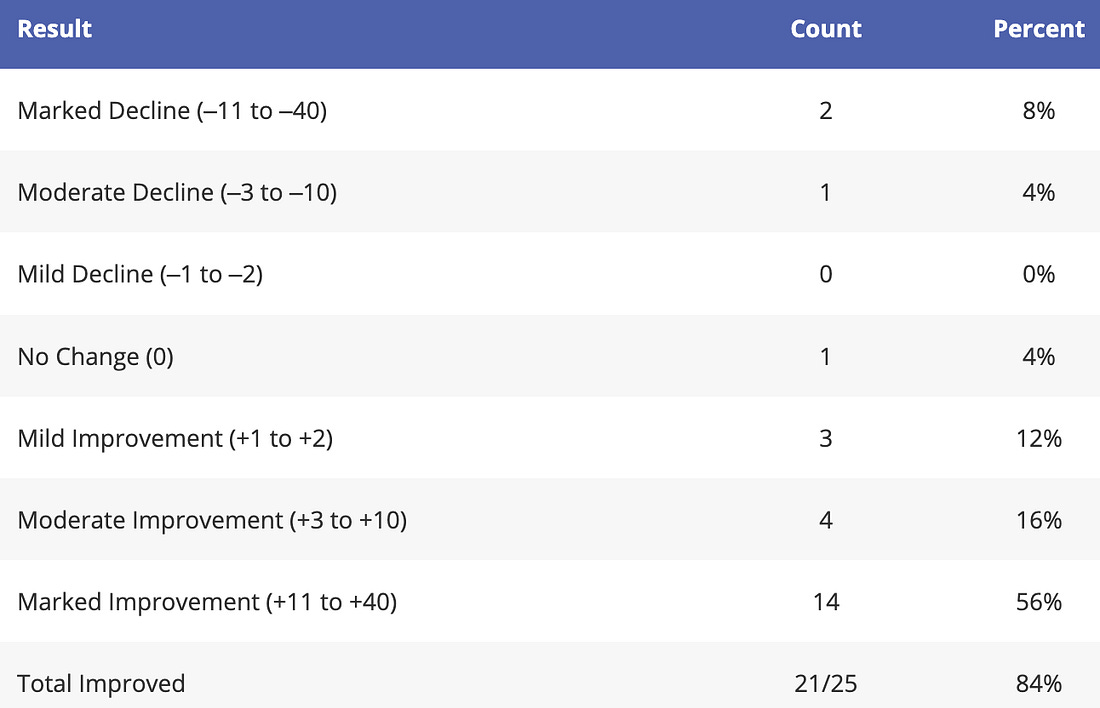
Most importantly, as the previous chart showed, his model worked. Beginning with a 2018 report of 100 patients from numerous providers whose cognitive decline was reversed by this model, a pilot study (completed in 2022) was able to show these remarkable case reports could be replicated in a controlled manner:
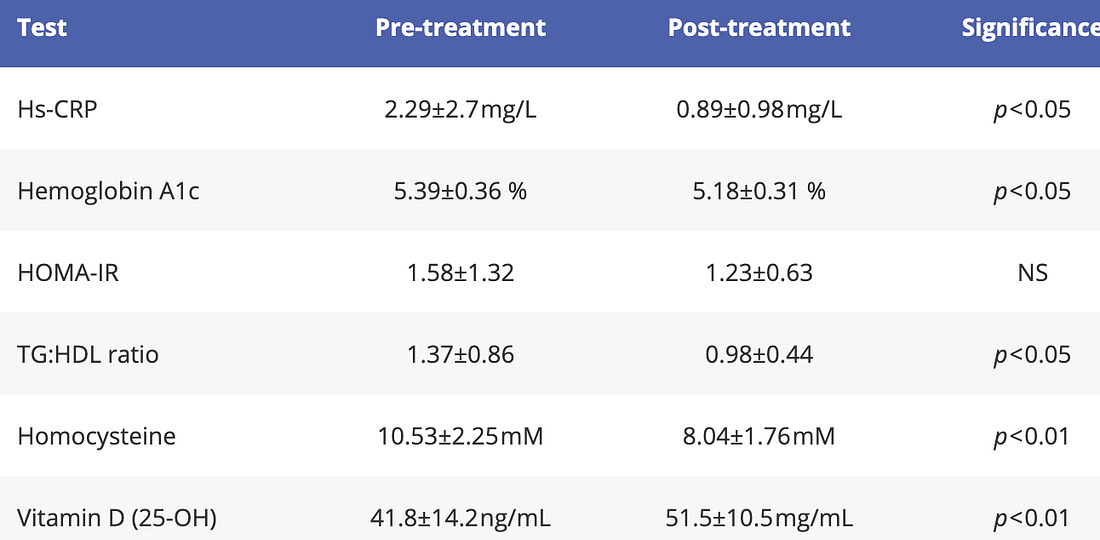
Likewise, he showed these improvements correlated to simple biochemical improvements:
Additionally, in 2024, he published a detailed set of case histories of patients who had remarkable responses to this protocol, and since his protocol was popularized, neurologists around the country he trained have begun administering it, often with significant success.
What Causes Alzheimer’s Disease?
This mirrors the three hats worn by the multitalented molecule, amyloid-beta, which is derived from APP. It is part of the inflammatory response and can function as an antimicrobial agent (thus it is part of your body’s ability to fight infections); it responds to inadequate levels of hormones, vitamins, nutrients, and other supportive (or trophic) factors by downsizing the more expendable synapses; it is part of the protective response to toxin exposure—for example, binding very tightly to metals such as mercury and copper [due to its negative charge].
In Bredesen’s model, there are multiple distinct types of Alzheimer’s disease, reflecting different underlying causes. The original three subtypes have since been expanded to at least five, each representing a different biological driver of cognitive decline. They are as follows:
• Type 1 – Inflammatory: This form is driven by excessive inflammation, often metabolic or infectious in nature. Chronic activation of the immune system—due to factors such as insulin resistance, a poor diet, a leaky gut, or latent infections—leads the brain to engage in protective downsizing by removing synapses and neurons that are less essential for immediate survival. This subtype often presents with classic Alzheimer’s memory loss and typically develops in the sixties to seventies. However, in individuals with substantial genetic risk (e.g., APOE4 carriers), it may appear earlier—in the late forties to fifties, or in the late fifties to sixties for those with a milder genetic predisposition.
• Type 1.5 – Glycotoxic: Sometimes referred to as a hybrid of Types 1 and 2, this subtype arises from insulin resistance and chronically elevated blood sugar. It leads to both inflammatory and trophic deficiencies, and is driven by glycotoxicity and the accumulation of advanced glycation end products (AGEs), which impair cellular function and synaptic integrity. It typically appears in the late fifties to sixties and is especially common in individuals with prediabetes or metabolic syndrome.
Note: the enzyme the body uses to break down insulin (which is nearly always chronically elevated in those who have metabolic syndrome) is the same enzyme it uses to break down amyloid plaques. Likewise, because elevated insulin levels and metabolic dysfunction play such a key role in Alzheimer’s, this has led many to refer to it as “type 3 diabetes.”
• Type 2 – Atrophic: This type is caused by deficiencies in nutrients, hormones, and other factors that provide trophic (supportive) signals to brain cells. These include vitamin D, thyroid hormone, estrogen, progesterone, testosterone, and brain-derived neurotrophic factor (BDNF), among others. The resulting lack of neuronal support triggers a similar downsizing mechanism seen in Type 1. Type 2 tends to emerge about a decade later than Type 1 and may occur alongside it, particularly in individuals experiencing both inflammation and hormonal/nutritional decline.
Note: I believe that in many cases, functional nutritional deficiencies result not from a lack of nutrients, but rather from a lack of fluid circulation that prevents those nutrients from reaching the cells. For this reason, I find that better results are sometimes seen from improving fluid circulation rather than aggressively increasing supplemental nutrition.
• Type 3 – Toxic: This subtype results from exposure to toxic substances that directly damage neurons. Common culprits include biotoxins, such as mold-derived mycotoxins (from water-damaged buildings—which is a huge issue), chronic infections (including Lyme disease), heavy metals (like mercury and lead), and industrial or household chemicals.
Note: the exact infectious agents are a matter of debate. For example, we’ve found that Cytomegalovirus, and Human Herpesvirus 6, can periodically cause cognitive decline, and once an appropriate antiviral is administered, a significant improvement is observed. Likewise, many believe Lyme bacteria within the brain is one of the most common infectious causes of cognitive decline and frequently treat it to address the condition. Bredesen, in his workhighlights the importance of Herpes simplex-1 virus, Lyme disease (a spirochete bacterium), P. gingivalis (an oral bacterium), and various fungal infections (mold toxins are notorious for causing cognitive impairment at all ages). Others also emphasize the importance of oral spirochete bacteria, which can travel into the brain.
Unlike Types 1 and 2, which involve more selective and adaptive brain responses, Type 3 causes widespread and often unpredictable neuronal death. It typically occurs earlier in life—often between the forties and sixties—and is less strongly associated with genetic risk factors, such as APOE4. Cognitive decline in this type is frequently accompanied by psychiatric symptoms, sensory changes, or executive dysfunction (e.g., difficulty with math, organization, executive tasks), rather than the more classic early Alzheimer’s memory loss. This type typically cannot be reversed unless the source of toxicity is identified and removed.
Note: I believe some of the most important neurotoxins to avoid are pharmaceuticals, and when I meet elderly individuals who have preserved their mental clarity, many report having largely avoided pharmaceuticals throughout their lives. Some of the most common problematic medications for brain health include certain high blood pressure medications (because they lower cerebral perfusion), statins (as they inhibit the production of compounds essential for brain function), acid reflux medications (which interfere with the absorption of vital brain nutrients—making it critical for everyone to have adequate stomach acid), antidepressants, antipsychotics, benzodiazepines, antihistamines (since, like many sleeping pills, they block restorative sleep), and anticholinergics (such as those prescribed for incontinence).
Additionally, after creating the initial list, he later created two more types:
• Type 4 – Vascular: In this form, chronic restriction of cerebral blood flow—due to factors such as hypertension, atherosclerosis, or small vessel disease—leads to gradual neuronal injury and cognitive decline. This vascular insufficiency deprives neurons of oxygen and glucose, impairing their function and survival. Type 4 often appears later in life (typically in the seventies or beyond) and may overlap with other subtypes. It tends to affect processing speed, attention, and executive function rather than memory alone.
• Type 5 – Traumatic: This subtype is associated with a history of brain injury—either a single significant concussion or multiple smaller, repeated head traumas. It is especially common in athletes and military veterans (although we also see it in less concussion prone individuals). The trauma sets off a cascade of inflammation, tau accumulation, and blood-brain barrier disruption, leading to chronic cognitive and emotional dysfunction. Symptoms can emerge years or even decades after the injuries, and they often include impulsivity, emotional instability, and executive dysfunction—with the best example of this being the dementia frequently seen in professional football players (which for decades the NFL covered up).
Note: there are a variety of causes of dementia. While Alzheimer’s is the most common, other forms such as frontotemporal dementia and vascular dementia also frequently occur. In many cases, the exact type of dementia one is diagnosed with is not always correct. One study found 30.2%-56.7% of those diagnosed with AD did not have it, an autopsy study found 12-23% did not have it, and a study found 63% of those with Alzheimer’s also had another dementia causing disease process within their brain (an issue that increases with age, further increasing the difficulty of accurately diagnosing dementia). However, since each of these diseases shares a similar process that causes their formation, it should be understood that what is described here often applies to treating forms of dementia as well as Alzheimer’s.
I generally agree with this list, and hesitate to disagree with it as he has much more experience in this area than I do. However, over the years, I have met numerous gifted physicians who have had varying degrees of success in treating dementia, in many cases with protocols that showed significant improvement.
From that experience, while I have seen many compelling models provide results, I have concluded that the primary issue is poor fluid circulation to the brain and poor fluid drainage from it, as this essentially explains all the other datapoints I’ve come across and frequently yields the most direct results for patients.
Note: while nutrition is important, I believe that in many cases, functional nutritional deficiencies result from insufficient blood flow to transport the existing nutrients to the tissues. For this reason, in many cases, I find that improving circulation rather than loading up on nutrients is an ideal treatment strategy.
More importantly, I find the same pathological processes that are at work in dementia are commonly seen in many other challenging chronic illnesses, and hence view the epidemic of Alzheimer’s disease to be yet another manifestation of systemic issues giving birth to a wave of chronic disease in our society, rather than an independent isolated problem.
Zeta Potential and Alzheimer’s
Whenever particles are mixed into a solution, they frequently become suspended (rather than sinking to the bottom or floating to the top). This results from each particle being repelled enough from the others that they separate and distribute evenly throughout the fluid (rather than clumping together). This process of colloidal suspension is greatly influenced by the surrounding charges (as like repels like). In most living systems, the greater the negative charge present, the more the colloids will be dispersed.
Conversely, when zeta potential is impaired, a variety of ailments will emerge from the congestion and thickening in the body’s fluids, such as frequent and damaging vaccine-induced microstrokes (which result from blood cells clumping together and obstructing the smallest vessels).
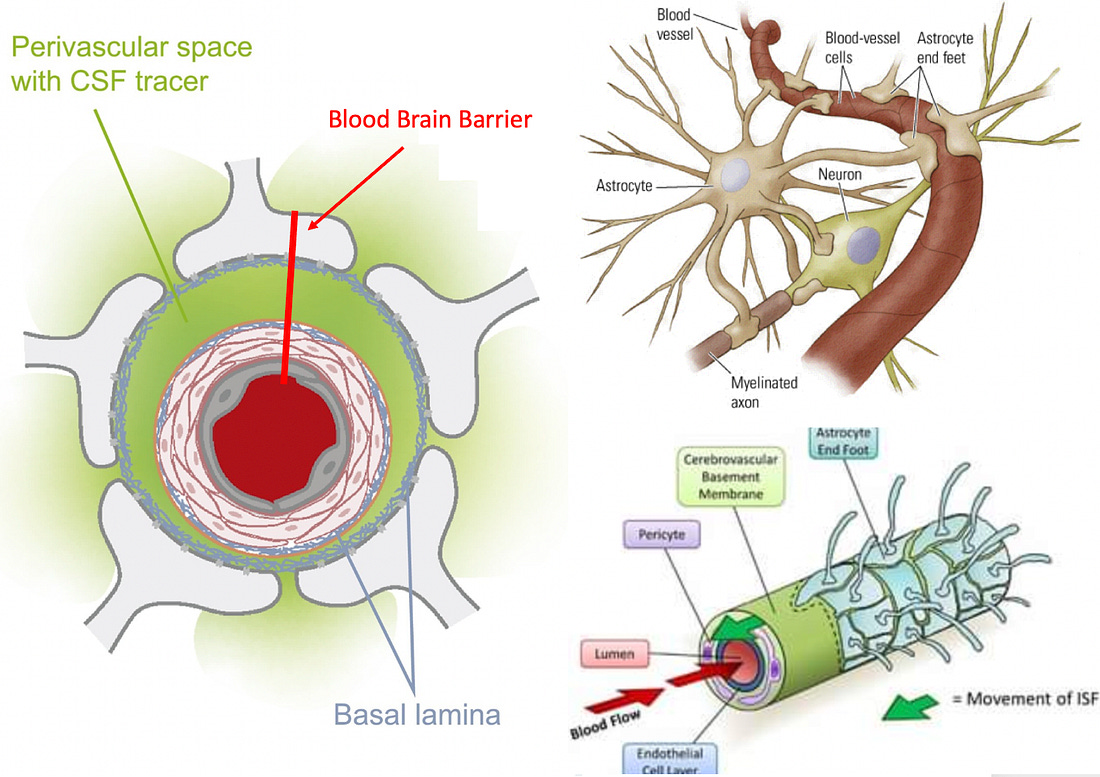
One of the most consequential fluid agglomerations is that of the lymphatics, the drainage system of the body (which amongst other things, is what removes products of inflammation from tissues such as those that damage brain tissue). The brain’s lymphatics (the glymphatics) are particularly vulnerable to this issue as rather than having specialized lymph vessels, its lymphatics exist in a perivascular space within the blood-brain barrier (a structure which is frequently disrupted in neurological illnesses such as Alzheimer’s, COVID-19 and most likely spike protein vaccine injuries—although it may be a while before someone will risk their career to research that).
Since this space is hidden between the feet of the astrocytes and the walls of the blood vessels and only expands during the night when you sleep as the astrocytes pull their feet back to support glymphatic drainage (a key reason why proper sleep is vital for preventing AD), it was not discovered until 2013. The structure of this system is important to understand because the only pump it has are the external walls of the blood vessel, and it is thus highly vulnerable to lymphatic agglomeration obstructing its flow or pathologic changes to the adjacent blood vessels that reduce their pumping motions.
Many different neurodegenerative disorders, especially those of aging, are associated with impaired glymphatic drainage (for example, traumatic brain injuries reduce glymphatic drainage, which helps to explain why experiencing a second concussion prior to the healing process completing can be so devastating and their association with Alzheimer’s). In the case of Alzheimer’s, the brain relies upon the glymphatic system to remove the neurotoxic and inflammatory agents linked to AD, along with its pathologic proteins (e.g., amyloids), so disabling this system (either directly or temporarily through sleep deprivation), in turn, increases the levels of those proteins by reducing their clearance.
Most importantly, in the same way cognitive impairment worsens with age, zeta potential decreases with aging (which I believe ultimately results from the kidneys gradually losing the ability to expel harmful positive ions and retain beneficial negative ones), and I know a few practitioners who had incredible results treating (or preventing) dementia simply by restoring the physiologic zeta potential of their patients.
Furthermore, in the same manner that physiologic zeta potential decreases with age, glymphatic drainage also decreases with age. As this decrease occurs in conjunction with the increased incidence of neurological degeneration with aging, the glymphatics have been argued to be the shared pathway for many of those disorders, which I would argue also suggests zeta potential is a key concern.
Note: I strongly believe one of the triggers for amyloid misfolding is a loss of zeta potential (as negative charges stabilize suspended proteins rather than causing them to clump together). In turn, there has been considerable controversy regarding whether aluminum is associated with Alzheimer’s. Studies have been put forward suggesting it is not (Bredesen for example, believes the evidence is sufficient to link mercury but not aluminum to Alzheimer’s), while others suggest it is and have provided data that it can be found within amyloid plaques. Presently, my opinion is that negatively charged amyloid has a high affinity for aluminum, and likewise, as aluminum is a highly effective agent for denaturing and precipitating proteins (due to its effect on zeta potential) and I suspect aluminum induces amyloid proteins to misfold and aggregate into plaques.
Additionally, as I highlighted in this article, a good case can be made that our entire understanding of cardiovascular disease is incorrect, as cholesterol, which is viewed as the cause of heart disease, actually is a patch that functions to repair already damaged arteries (a situation again similar to Bredesen’s amyloid model). As such, treating heart disease is often a question of reducing damage to the blood vessels, and then restoring them to their normal function.
In turn, there is a significant overlap between blood vessel damage and cognitive decline, something I would argue is a result of insufficient blood reaching the brain along with both conditions sharing many similar causes (e.g., diabetes not only chronically overwhelms the amyloid disposing enzyme but also damages blood vessels and hence reduces blood flow).
As such, similar agents have similar effects on both, such as the COVID vaccines (which not only caused heart issues, but also frequently caused cognitive impairment in healthy adults and in many cases, caused elderly patients to develop rapidly accelerating cognitive decline or dementia).
Note: while the most dramatic effects were seen with the COVID vaccines, many readers here have shared seeing an older relative cognitively decline after an influenza or pneumonia vaccine (which I believe results from their adverse effect on zeta potential).
Additionally:
•Physical inactivity is strongly linked to dementia (e.g., large reviews have found between 40-45% of dementia could be prevented or delayed with regular physical activity1,2). I believe this is due to physical activity being vital for the fluid circulation in your body, particularly within the lymphatic system.
•About twenty years ago, a theory emerged that multiple sclerosis was due to poor drainage of the jugular vein (causing toxins to be retained in the head), which was then treated by stenting the vein open. The success of this approach led to its use for other complex neurological illnesses (e.g., Lyme disease), and prior to the FDA banning the practice, I came across numerous reports of its effectiveness (e.g., from Dietrich Klinghardt)—again illustrating the importance of ensuring proper drainage from the head.
Sleep and Dementia
As many of you know from personal experience, sleep loss is well recognized to cause brain fog and cognitive impairment (e.g., this study demonstrated that sleep deprivation worsened auditory processing and responses on neurophysiological tests).
This process is particularly consequential in the elderly (who are widely recognized to be more susceptible to memory loss and cognitive impairment), and likewise more likely to suffer from impaired sleep as they age.
As this review paper shows, a significant body of research ties poor sleep (especially if chronic) to dementia. For example:
- A study compared 105 older women with sleep-disordered breathing (which impairs sleep) to 193 without it and found that sleep-impaired individuals were 71% more likely to develop mild cognitive impairment and 104% more likely to develop dementia.
- In one study, 737 older adults initially without dementia received annual measurements of their sleep quality, their cognition, and the presence of Alzheimer’s Disease (AD). After 6 years, individuals with poor sleep (high sleep fragmentation) were found to have a 22% increase in their risk of AD, with those who had the worst sleep fragmentation having a 50% increase.
- A study recruited 346 patients with normal cognition, averaging 75.9 years of age, 80 of whom had insomnia. It found that those with insomnia were 139% more likely to develop AD.
- Sleeping disorders are prevalent in AD. For example one study found that the seven most common sleeping disorders occurred in between 50.0% to 65.5% of those with AD (which was 2.0-4.46 as frequent as that seen in patients without AD).
Furthermore, many studies have directly tied poor sleep to the pathogenesis of AD. For example:
•A remarkable 2020 study of 32 individuals without cognitive impairment who received an average of 6.1 months of sleep assessments and 3.7 years of PET scans (a non-invasive way to measure Alzheimer’s plaques in the brain) found that disrupted sleep caused an accelerated accumulation of Alzheimer’s plaque and forecasted the development of dementia. These results are significant as most adults at this stage do not recognize the damage accumulating in their brain, which will inevitably lead to dementia.
Note: one of the unfortunate things about AD is that the presence of one of the misshapen proteins found in it (tau) has been linked to impaired sleep quality, while the other, β-amyloid has been linked to losing the ability to recognize one is suffering from impaired sleep. These facts, combined with the 2020 study help to illustrate why AD can be so insidious and seem inevitable once it’s snuck up on someone. Likewise, in the same way poor sleep impairs the retention of long-term memory, AD disease plaques do as well.
•Deep sleep has been shown to mitigate the cognitive impairment created by Alzheimer’s plaques.
It hence should come as no surprise restoring healthy sleep was a core component of Bredesen’s program, and likewise, remarkable that it’s only been in the last few years that healthy sleep has begun being considered as a way to head off dementia.
Note: sleeping pills block restorative sleep, and have a variety of issues (e.g., they make users 2-5 times as likely to die1,2). Regarding dementia, multiple studies have found that sleeping pills increase the risk of it by 17-84%.1,2,3,4
The Life of Cells
One of the things I continually marvel at about nature is not only the ability of a species to genetically adapt to its environment, but the inherent adaptability each organism has within its own lifespan to adapt to its environment. Within the human body, there are many systems that are designed to change based on the needs of one’s environment (e.g. this is why weight training creates larger muscles), and among the most adaptable is the nervous system.
So, at any given moment, neural circuits that support certain activities are reinforced, while other circuits are pruned and eventually disabled, a process that allows the nervous system to adapt to the complex needs of its environment. At the same time, many complex neurological and psychiatric disorders arise from a momentum being established where dysfunctional neurological circuits perpetually reinforce themselves.
For these disorders to be treated, a momentum must instead be established behind a healthy circuit (for those interested, this is the best book I have seen on that subject). This momentum is a key reason why it is so important to have healthy thought patterns and regularly actively exercise your brain (another core component of programs for preventing Alzheimer’s). If you do the opposite (e.g., watch TV all day), dysfunctional patterns can become established habits, while neurological damage occurs as parts of the brain you need but under utilize are pruned away.
A key way the brain accomplishes this adaptability is by eliminating neurons that are no longer deemed essential. Bredesen’s theory of Alzheimer’s is that it results from the balance between preserving and eliminating neurons being shifted towards eliminating them, which inevitably will result in cognitive decline.
Within Bredesen’s model, the amyloid protein plays a key role in this process, as when it is initially formed as amyloid precursor protein (APP), it has the choice to be then split into two or four parts. If it is divided into two parts, those parts protect the neurological function in the brain. In comparison, if it is divided into four parts, the neurological function of the brain is damaged, and brain cells are eliminated. Interestingly, its splitting into four parts causes future APPs also to be split into four parts (which creates a downhill spiral). As a result, Brenden’s approach focuses on regaining a healthy momentum towards the two-part splitting while also providing the signals cells within the body require to survive.
The Cell Danger Response
One of the better models I have come across for understanding complex illness, the cell danger response, shows that in response to environmental stressors or pathogens, cells can enter a defensive metabolic cycle where they partially or fully “turn off“ (e.g. mitochondrial respiration and protein synthesis within the cell decline). The cell danger response is often observed in patients with chronic illnesses (e.g. fibromyalgia or childhood vaccine injuries), when looked for, is frequently observed following COVID-19 vaccine injuries, and in many cases, produces remarkable results for chronic illnesses once addressed.
In parallel, one of the more promising approaches to treating cognitive decline also targets this process of the cell turning off by disabling what is referred to by its proponents as the “integrated stress response.”
“The principle that blocking protein synthesis prevents long-term memory storage was discovered many years ago. With age there is a marked decline of protein synthesis in the brain that correlates with defects in proper protein folding. Accumulation of misfolded proteins can activate the integrated stress response (ISR), an evolutionary conserved pathway that decreases protein synthesis. In this way, the ISR may have a causative role in age-related cognitive decline.”
When tested, an ISR inhibitor was found to restore the structure and function of cells within the brain and to improve a variety of age-related memory deficits in mice.
Likewise, within regenerative medicine, one of the most commonly encountered issues is that cells become senescent and cease dividing (in other words, the cells partially turn off). This is addressed by providing signals to the cells to come back to life and resume their division.
Note: frequently, cells receiving a signal to turn off precedes them undergoing programmed cell death. As Bredesen’s model highlights, neurons within the brain have receptors (termed dependence receptors), which if not repeatedly stimulated, will initiate that cycle, and amyloid precursor protein, if split into four parts, blocks those receptors from being stimulated, thereby triggering programmed cell death.
Many other factors can also trigger programmed cell death of neurons. For example, following vascular strokes, many cells in the brain will turn off, and if not brought back (e.g., with DMSO) will frequently die, resulting in long-term damage from strokes.
Another common situation that results in brain cells turning off is anesthesia (which is what has to happen when they put you out). This is problematic because some neurons in the brain will not wake up after surgery is completed, and once looked for, it is often possible to track cognitive decline emerging after the anesthetic was applied at a time that is often too far out (e.g. six months later) for the patient to recognize an association between those two events (although some evidence now exists for this association).
This is primarily an issue with inhaled anesthetics (Bredesen does list previous anesthetic exposure as one of the many toxin exposures he evaluates for), and can be avoided if agents such as IV Ketamine or Midazolam (Versed) are used instead for anesthesia—which some anesthesiologists will agree to.
Note: to some extent, this can also be mitigated by specific B vitamins before and after surgery.
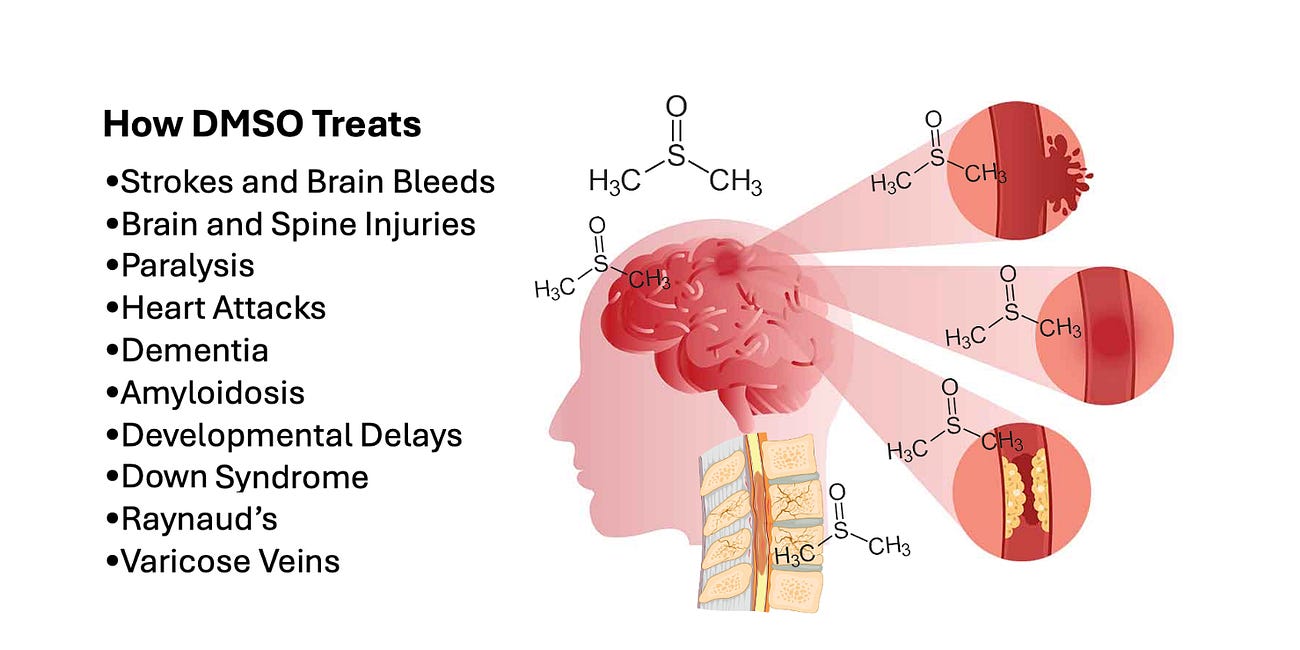
DMSO and Dementia
Dimethyl sulfoxide (DMSO) is a naturally occurring compound found throughout nature, which was initially used as a chemical solvent. It then entered medical use after the company producing DMSO in America (to meet the industrial need) noticed that it also had remarkable therapeutic properties. As people became aware of what DMSO could do, its popularity spread like wildfire, and within a few years, it became the most demanded drug in America. Sadly, the FDA, overwhelmed by the number of new drug applications they were receiving and members of the public (who did not want to wait for approval), using DMSO on their own, decided to address this massive regulatory challenge by banning DMSO.
This led to decades of resistance against the FDA’s ban by not only the desperate public, but also Congress and large segments of the medical community (which resulted in thousands of independent unfunded studies being published on the therapeutic properties of DMSO). Curiously however, while the FDA banned all but one medical use for DMSO and forbid companies from sponsoring research on it, they eventually permitted it to be mixed with a variety of (patentable) pharmaceutical products—resulting in DMSO ultimately being classified as a safe and inert ingredient that exists within a large number of approved pharmaceutical formulations.
Note: throughout this period, the FDA did all they could to find any evidence that DMSO was dangerous (to justify their extremely unpopular ban), but due to its low toxicity, the FDA never could, even when people were subjected to the highest possible topical doses (covering the whole body in DMSO multiple times per day). Presently, the only evidence of toxicity for DMSO (discussed further here) can be found [intermittently] in cell studies where cells are kept for days at a time in concentrations of DMSO hundreds of times higher than can occur within the body (and hundreds to thousands of times higher than toxicity thresholds for most commonly used drugs or vitamins). Likewise, globally, since 1960, I have only been able to identify three deaths that have been associated with DMSO, where in all three cases, there was never a consensus if DMSO was the cause of death (whereas many widely used drugs kill dozens of people each day).
Eventually, the FDA lost its ability to ban DMSO due to a 1994 law being passed (in response to the public getting fed up with the FDA raiding natural medicine providers at gunpoint) and Congress taking away its ability to regulate natural supplements. Sadly, at this point, decades of campaigns against DMSO had made the therapeutic use of it become forgotten, so once it was legalized, minimal knowledge of it existed outside of its pharmaceutical uses, and hence DMSO was only used in small segments of the natural health community.
Note: the entire history of DMSO is detailed here, while the information on it’s safety is detailed here.
For this reason, we made the decision to try to bring awareness to DMSO with this newsletter (by having now presented well over a thousand summarized studies here). This inspired many to try DMSO, and over the last year, thousands of readers have reported remarkable improvements from DMSO (which I compiled here) that are very similar to those which emerged in the early days of DMSO before the FDA buried it. Some include:
My uncle’s wife has dementia and has been unable to speak for over a year. My mom recently visited them and told them about DMSO. He began to give his wife DMSO orally. After two week she began to talk again.
I read the article and began giving it to my 93 year old mother in her juice every morning the end of November. She has had some form of dementia for over 15 years. In the last year or so she would get sundowners really bad and could not follow instructions.
Since taking the DMSO, she no longer suffers with sundowners. She is more “with it” and can communicate and laugh with us. Her personality is back. She is crossing her legs again and lifting her pinky finger when drinking her coffee. It’s a lot of little things that make a difference. She is able to understand when I am asking her to use the bathroom. She is more cognitive and has started coloring in her coloring books again. I have been telling everyone about it.
I deeply appreciate your posts on DMSO. You helped bring spontaneous interaction back into the life of my father with Alzheimer’s. As well as many other people I have educated about it’s uses God bless you.
One of the key reasons DMSO has such a low toxicity (detailed here) is due to it being able to protect cells from a variety of otherwise lethal stressors (e.g., blood loss, radiation, freezing, sound shockwaves—of which freezing is the most popular application)—something I attribute to it greatly improving blood flow throughout the body, it reducing inflammation (significantly reducing the longterm impact of otherwise lethal stressors), and DMSO reviving cells trapped or frozen within the cell danger response.
Note: DMSO’s anti-inflammatory and antioxidant have been properties have been repeatedly proposed to account for its ability to treat Alzheimer’s disease.1,2
These protective properties are particularly valuable for the (fragile) central nervous system, and one of DMSO’s most remarkable properties is its ability to treat strokes, brain injuries, and spinal cord injuries, which otherwise are often lethal or permanently disabling.
As such, while DMSO has a variety of paradigm shifting uses (e.g., it is one of the safest and most effective pain medications available—with many readers attesting DMSO immediately erased years of incurable pain), my specific motivation for spending the last year of my life on this series was due to how unjust I felt it was that its use was restricted from patients with severe neurological injuries.
For that reason, I spent the last two months reviewing a large body of research to revise the original article I wrote on the topic (which can be read here).
Note: I compiled numerous reports I’ve received from readers about DMSO treating a stroke here.
DMSO’s ability to heal the nervous system (and its ability to address many of the root causes of dementia), in turn, also extends to it being able to reverse cognitive decline (which may in part result from its being remarkably effective at eliminating insoluble amyloid deposits and amyloid-β aggregation). For example, in animal studies:
•When rats had their carotid arteries surgically modified to significantly reduce the amount of blood going to their brain, after 3 months, it was found that DMSO prevented both the neuronal damage and the significant loss of spatial memory and learning that otherwise resulted from that chronic loss of cerebral blood flow.
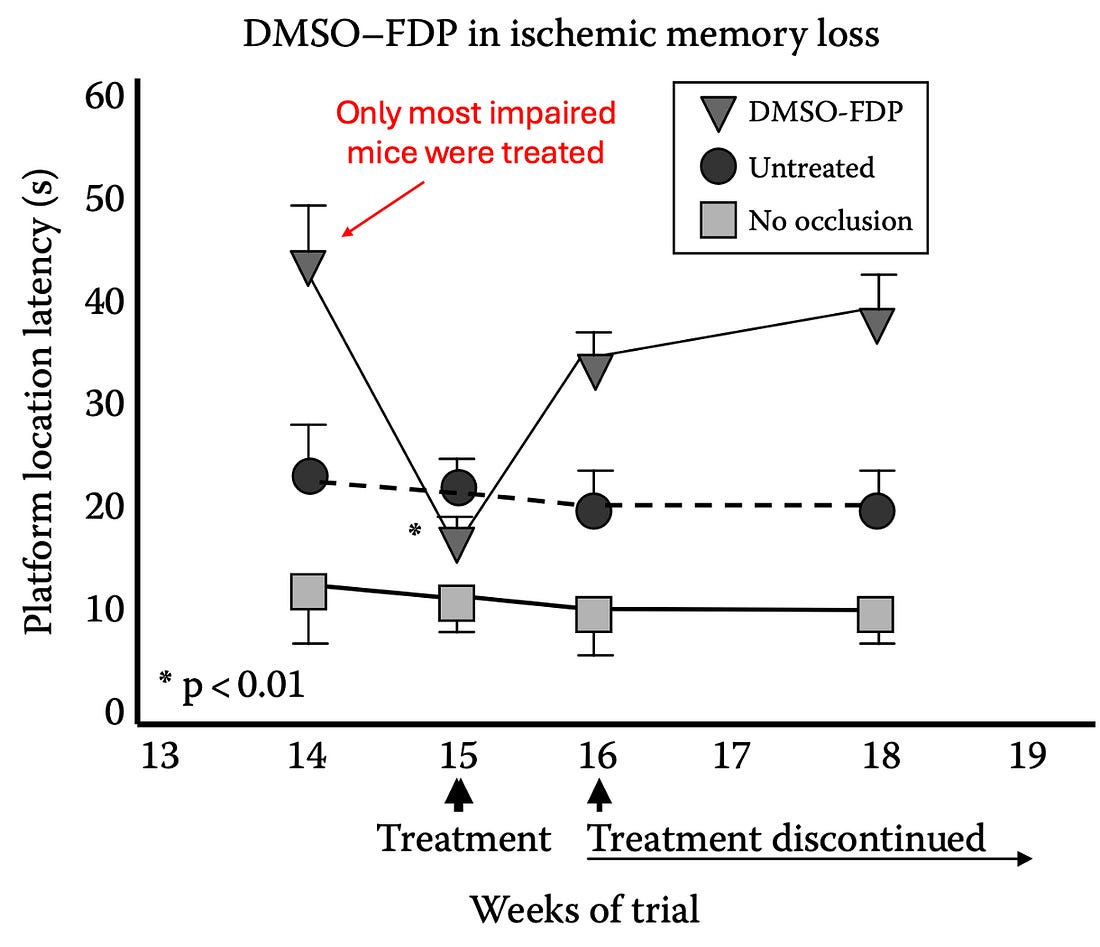
•In a similar study, rats 14 weeks old were subjected to either permanent bilateral carotid artery occlusion or sham occlusion (mimicking the chronic vascular impairments many experience with increasing age). Then they tested the rats for visuospatial memory function. After 14 weeks, four rats who had shown persistent and severe memory impairment received DMSO and FDP for 7 days, which improved their memory by 54%, almost reaching the cognitive function of the controls. Unfortunately, this improvement was partially lost once DMSO-FDP was discontinued.1,2
•In rats, daily IV DMSO (for 2 weeks) counteracted memory impairment induced by intracerebroventricular STZ infusions, as shown by improved performance in behavioral and memory tests (e.g., Morris water maze). In a similar study, DMSO and Ginkgo biloba extract improved learning and memory in Alzheimer’s disease model rats (induced by β-amyloid 25-35 hippocampal injection), reducing escape latency and searching distance in the Morris water maze.
•0.01% DMSO was mixed with the drinking water of young (3-4 months) mice genetically engineered to have early onset Alzheimer’s. DMSO was found to mitigate the visual declines and ELM-RPE thickening within the retina seen in the prodromal phase of Alzheimer’s disease (with the benefits being comparable to those seen with R-carvedilol). Additionally improving that thickening was assumed to indicate that DMSO enhanced the energy dependent transportation of water out of the eyes.
•In mice genetically engineered to have Alzheimer’s disease [AD], DMSO has been shown to increase neuronal density in the hippocampus (a brain region vulnerable to AD) and enhance their spatial memory and smell (while decreasing their anxiety), along with normalizing hippocampal hyperactivation and modulating the NMDA receptor.
Note: DMSO has also been shown to greatly delay (by 48-98%) the paralysis caused by amyloid beta in C. elegans (one of the most popular organisms for aging research) and to extend the lifespan of C. elegans by 23.0-24.4%. The researchers attributed this delay in paralysis to DMSO modulating neurotransmission (e.g., DMSO is an acetylcholine esterase inhibitor, a therapeutic strategy also used to treat Alzheimer’s).
•In rats with rotenone-induced Parkinson’s, DMSO significantly improved the morphological integrity of pyramidal cells and Nissl bodies in the hippocampal CA1 and CA3 areas, counteracting the neuronal damage caused by rotenone. It also suppressed both inward (depolarizing) and outward (repolarizing) currents, enhanced tetanic depression responses, and strengthened inhibitory signaling in response to high-frequency stimulation (thereby counteracting the hyperexcitability and excessive activity induced by rotenone, protecting the hippocampus from excitotoxicity).
Note: IV DMSO is one of the few therapies I have come across which can halt Parkinson’s. To some extent oral DMSO helps as well (e.g., see this reader’s comment).
•In hamsters with scrapie infections (a neurodegenerative prion disease from abnormal protein aggregates), DMSO added to their water prolonged disease incubation time and delayed the accumulation of protease-resistant PrPSc in the brain. Additionally, in the way DMSO helps treat amyloidosis, DMSO increased the excretion of protease-resistant PrP in the urine
Note: DMSO was also found to increases the activity of lysosomal alkaline phosphatase (ALP) by 20%. As lysosomes eliminate cellular waste (e.g., damaged organelles, misfolded proteins, and other cellular debris), this likely increases the elimination of the toxic aggregates that contribute to neurodegenerative diseases like Alzheimer’s or Parkinson’s (particularly since DMSO also increases the permeability of cell membranes and hence the ability of cells to eliminate waste products). Likewise, by breaking down unneeded cellular materials, the energy they contain can be made available for cellular metabolism (which is often dysfunctional in neurodegenerative diseases).
•Lurcher mice are used to study olivary and cerebellar disorders because their Purkinje cells can’t survive (e.g., by 30 days of age their walking is grossly abnormal). When these mice received DMSO, it prevented the age-related deterioration of certain cognitive functions (e.g., memory and spatial learning abilities)
Most importantly, these results have been replicated in humans:
•18 patients with probable Alzheimer’s were treated with DMSO and tested regularly for nine months, with great improvements being noted after only three months of treatment, and becoming especially noticeable after six months of treatment. Areas of improvement included memory, concentration, and communication alongside a significant decrease of disorientation in time and space.
•Another study evaluated 104 elderly adults with organic brain disease due to cerebrovascular diseases (e.g., a previous stroke, cerebral embolism or a hardening of the arteries of the brain), a previous head injury, senility, or degenerative disease (e.g., Parkinson’s, hyperthyroidism or epilepsy). They received two DMSO mixes, Merinex (DMSO with amino acids) and Ipran (DMSO with vasoactive substances), typically alternating between the two, and for the majority of the time as an injection, and a minority of the time orally (with the fastest results occurred if both routes were used simultaneously), all of which resulted in remarkable improvements. To quote the author:
The DMSO amino acid therapy is undoubtedly valuable in the treatment of numerous organic cerebral diseases. At the same time, thanks to the improved cerebral blood irrigation achieved by DMSO used in combination with vasoactive substances, a highly favorable effect on the psychic and somatic functions of senile patients was achieved.
•A Chilean study evaluated 100 patients with cerebrovascular diseases (e.g., a previous stroke, cerebral embolism, or a hardening of the arteries of the brain), many of whom were senile, who received DMSO orally and through intramuscular injections over the course of 50 days. It was noted that their coronary heart disease (i.e., atherosclerosis) and high blood pressure had a good improvement in 74.35% of DMSO recipients, a fair response in 21.77%, and no response for 3.88%. The neurologists overseeing these patients remarked that:
“Recovery from the general symptoms was positive; there were favorable changes which were reflected in a feeling of well being, the recovery of agility, changes of mood from depressed to gay, improvement of sleeping, and clearer speech. As regards the ‘focal’ results, accelerated recovery from hemiplegia and hemiparesia was registered. A speedier recovery of speech in cases of defined or indicated aphasia took place.”
As such, I would argue:
•DMSO’s ability to treat dementia suggests that many of its causes overlap with what DMSO addresses within the body (e.g., poor circulation, or cells trapped within the cell danger response).
•DMSO again illustrates how a widely available and affordable therapy has been withheld from the public to support the amyloid therapy market.
Treating Dementia
Since our focus in treating Alzheimer’s disease has been so directed at finding a blockbuster drug, many of the ideas laid out throughout this article remain almost completely unknown—a situation I would argue is analogous to the other neurodegenerative disorder overwhelming our society, autism (that shares many of the same root causes as dementia).
As such, there has been very little focus either on the simple things we can do to prevent dementia (e.g., mental activity, sunlight exposure, healthy sleep, exercise, improving metabolic health) or the already available treatments for cognitive decline —which in almost all cases precedes dementia (as they share the same causes, but are much easier to address when only cognitive impairment has manifested).
In the final part of the article, I will discuss each of those treatments (e.g., key nutritional therapies, therapies to resolve past concussions, ways to improve brain circulation or treat the cell danger response there), how to utilize them (e.g., for DMSO, restoring zeta potential), and our perspectives on other commonly used approaches (e.g., nicotine)…





Leave a Reply
You must be logged in to post a comment.